Autogenous Procedures for Implant Placement
Classification of the extraction socket determines what approach will be performed when an implant is planned for the site. Extraction sockets have been classified into three types based on the facial/buccal bone and soft tissue position (Eilan et al.):
- Type I Socket. The facial soft tissue and buccal plate of bone are at normal levels in relation to the cementoenamel junction of the pre-extracted tooth and remain intact postextraction.
- Type II Socket. Facial soft tissue is present, but the buccal plate is partially missing following the extraction of the tooth.
- Type III Socket. The facial soft tissue and the buccal plate of bone are both markedly reduced after tooth extraction.
Treatment of Socket Type 2

Soft tissue and facial bone loss limits the ability for immediate implant placement and may complicate eventual implant placement even at healed sites.
Type II sockets are often the most difficult to diagnose. These sockets can be very deceptive, as the gingival margin position is at the CEJ or slightly coronal or apical to it. Yet, the facial crest of bone is a distance apical to the gingival margin, leading to this type of socket being mistaken for type I.
Natural dehiscence is not uncommon, even though a healthy dentition is present. Frequently, the facial plate is absent as a result of vertical root fracture(s). When the natural tooth fails related to endodontic origin, the facial plate at the root may be partially or completely absent, hampering the placement of an implant at the time of extraction.
Various methods have been proposed for the treatment of simultaneous hard and soft tissue augmentation of extraction sockets, whether at the time of extraction or defects resulting from prior extraction sites. For Immediate Dentoalveolar Restoration (IDR) introduced by da Rosa, an autogenous hard tissue graft taken from the patients’ tuberosity is utilized. But, it may not be possible to harvest sufficient bone volume from the tuberosity, as this is dependent on what bone is present in this area in the particular patient. The IDR technique requires immediately placed implants with immediate provisionalization. Depending on apical defects and sagittal root position, primary implant stability may not be achieved in all cases.
Hard and Soft Tissue Augmentation
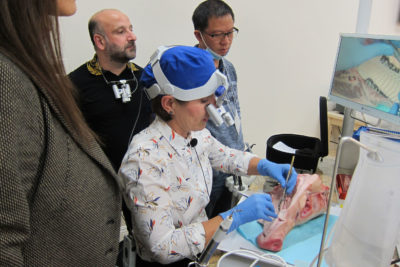
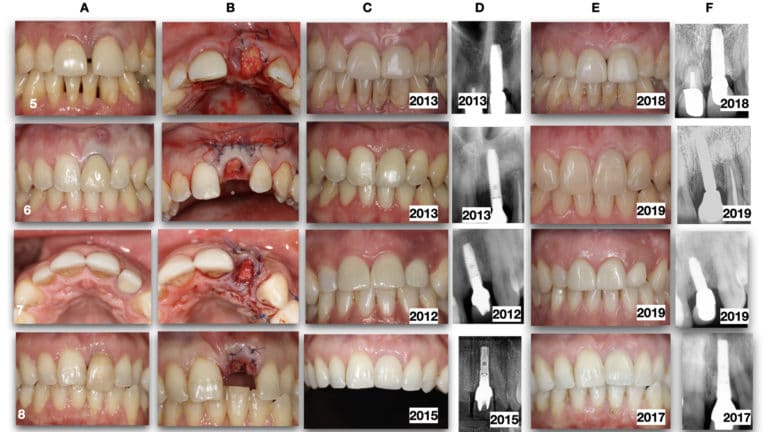
mIVAN technique is a technique for simultaneous hard and soft tissue augmentation at socket types 2 and 3 and at implant placement in the ridge with horizontal atrophy.
Grafting and a delayed implant placement approach may be required to provide sufficient bone to encompass and support the implant. Grafting needs may involve bone replacement and require soft tissue augmentation to achieve proper site closure. During the healing phase, additional soft tissue coverage is often necessary to contain the hard tissue augmentation. Soft tissue augmentation may also provide adequate attached gingiva for long-term periodontal health.

Simultaneously rebuilding the soft tissue with hard tissue augmentation of the extraction socket becomes difficult due to poor blood flow in the overlaying soft tissue graft. To circumvent this issue, a Vascularised Interpositional Periosteal Connective Tissue flap (VIP -CT) has been developed as an anteriorly based pediculated tissue of palatal submucosa. Its maintained blood supply allows graft survival on the poorly vascularized hard tissue augmentation placed at the same surgery. Fagan, 2008 described a procedure for simultaneous hard and soft tissue augmentation of facial bone wall missing sockets for implant site development. This technique, called IVAN (Interpositional Vascularized Augmentation Neogenesis), consists of hard tissue grafts, various barrier membranes, and closure with the VIP-CT. The advantage of IVAN over other previously described techniques is no coronal flap advancement is required. Loss of keratinized gingiva may result in coronal advancement of the flap as well as an esthetic discrepancy in the height of the mucogingival junction with adjacent areas, defective papillae, and incision scars.
Modification of IVAN technique (mIVAN technique):
A vestibular soft tissue tunnel is prepared to augment the buccal soft tissue and to provide VIP-CT with additional blood supply from that area. The addition of the VIP-CT underneath the mucosa (in the split-thickness tunnel) not only gives volume to the soft tissue on the facial aspect of the ridge but also improves gingiva color and texture (stippling) to yield a more natural end result following healing.
A vestibular soft tissue tunnel is prepared to augment the buccal soft tissue and to provide VIP-CT with additional blood supply from that area. The addition of the VIP-CT underneath the mucosa (in the split-thickness tunnel) not only gives volume to the soft tissue on the facial aspect of the ridge but also improves gingiva color and texture (stippling) to yield a more natural end result following healing.

Conclusion
The mIVAN technique allows preparation of the site for subsequent implant placement following soft tissue healing and hard tissue graft incorporation with the host bone, resulting in the quality bone to house the implant circumferentially in type II and III sockets. When extractions are performed without socket maintenance at the time of tooth loss, and a delayed implant placement approach is utilized (either due to the need for site healing or the patient’s financial decisions), this often leads to horizontal bone loss plus a defect on the buccal aspect of the ridge.
To Learn the Techniques Mentioned in this Blog.. Click Here