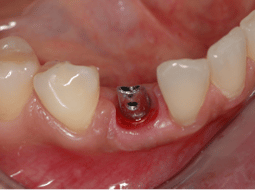
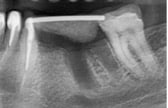
Fig 1a, 1b, 1c : Enough bone volume and soft tissue availability horizontally and vertically allowing implant insertion in a prosthetic driven position. Fig 1d : Esthetic final result imitating the adjacent natural teeth.
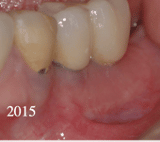
Fig 2a, 2b : Esthetic and functional results can be predicted and reproduced as much as enough hard and soft tissue are available, inserting the implant in a prosthetically driven position operated by surgeon and prosthodontist with certain skills in implant treatment.
Requirements for a long-term successful implant treatment
Regardless of the atrophy, disease, or injury of the site to restore, an adequate implant placement and natural esthetic appearance of final prosthesis require more than focusing on tooth or teeth to be replaced. The Implant surgeon as well as the prosthodontist, should consider a broad and complex set of interwoven factors before inserting the implant.
After tooth extraction it is most usual to have a depletion of the alveolar process that can affect the stability of the peri-implant soft and hard tissue through time of the replaced implant restoration. In the early 70s and 80s the original treatment protocols of implant treatment required fully healed alveolar ridges before implants placement. Eventually, these protocols were modified to include implant placement in fresh extraction sockets or in partially healed alveolar ridge predominantly for implants in the esthetic zone. However, immediate implant placement does not stop buccal bone and soft tissue remodelling following tooth extraction. Never less, risk of bone and soft tissue collapse may be reduced during immediate implantation by following very strict conditions like the presence, before extraction, of thick facial bone wall, thick tissue biotype, similar initial esthetic gingival level with the adjacent teeth and the implant positioning within the extraction sockets in a prosthetically driven insertion.
One of the crucial criteria to assess clinical success is not only to achieve esthetically acceptable peri-implant tissue but to maintain that tissue as long as possible under loading and through time.
Fig 3a, 3b, 3c : Reproducing esthetically and functionally missing natural teeth with implants is not enough. It is essential that this result last for a long time.
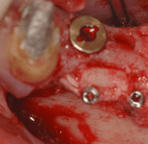
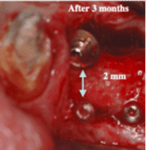
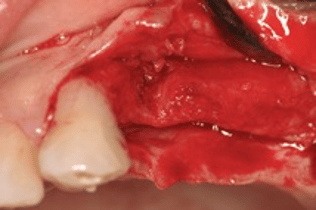
Fig 4a, 4b, 4c, 4d : A minimum 2 mm of hard and soft tissue thickness and width are essential to insure long term stability during functional loading . Notice the gingival recession on the natural canine after 8 years with the stability around the adjacent implant on the first premolar site (fig. 4.a & b).
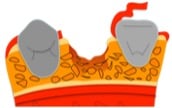
Appropriate horizontal bone level and thickness with adequate attached gingiva height and thickness surrounding the implant cervically was associated with diminished vertical bone resorption and by consequences less peri-implant mucosal recession. The adequate peri-implant bone sustains and stabilizes the soft tissues and in return a fixed soft tissue covering the underneath bone keep away the muscle activity and avoid the risk of biomechanical bone resorption.
The absence of implant facial bone is not the only situation associated with gingival recession problems; thin cortical bone surrounding the implant is subject to instability by itself and may not survive by lack of blood supply due to the presence of the implant blocking the blood vessels reaching appropriately this bone during healing phase. Thicker bone, characterized by a better blood supply, would be less susceptible to resorption.
Vertical facial bone stability has been related to thickness of the bone at the time of second stage surgery and prosthetic reconstruction. A minimum bone thickness of 2 mm has been recommended for more than 4 decades and still up to date with recent studies.
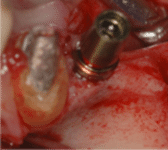
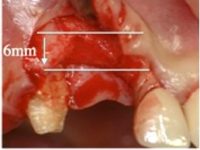
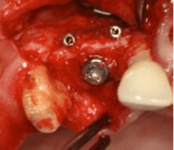
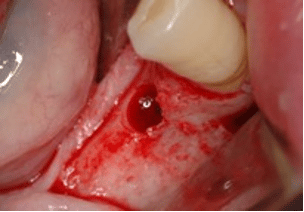
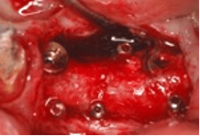
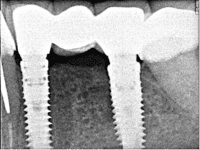
Fig. 5a, 5b : Less than 2 mm peri-implant bone cervically present higher risk of resorption on a short term even if the implant is totally covered by bone. Bone core harvested from implant bed site is regrafted buccally to increase thickness.
Fig. 5c, 5d : Results after 3 months of minimal invasive bone grafting simultaneously with implant insertion and appropriate soft tissue management .
If the presence and dimensions of peri-implant bone are key factors for ensuring esthetic peri-implant mucosal contours stability on a short or medium term, a fixed attached gingiva, with adequate thickness and width, covering this bone is essential to keep muscle activity on a distance and avoid bone resorption by time during function and provide a long-term peri-implant tissue contour stability.
When implant-supported prostheses were first used, a circumferential sealing by the connective tissue collar was considered crucial for maintaining peri-implant health. However, tissue vulnerability and resistance have been shown to depend on the epithelial barrier cells regardless of the presence or absence of keratinization.
Many studies showed that marginal bone loss at the one-year of follow-up after loading of dental implants with a thin and/or narrow width crest fixed mucosa (<2 mm) was significantly bigger than implants placed in a ridge area with a thicker fixed one. These observations clearly indicate that the thickness and the width of the fixed mucosa, whether keratinized or lining mucosa, is a key factor that will influence the degree of early peri-implant bone loss. Minimum of 2 mm in width and thickness of fixed mucosa is essential to predict a stable long-term bone and consequently stable gingival level.
Furthermore, in the esthetic zone, even if the implant is correctly positioned and well covered with at least 2 mm of hard and soft tissue, more soft tissue volume is still desirable because the tooth loss has led to a change in the alveolar ridge from a convex into a concave shape. If the implant is surrounded by plenty of bone, an increase in soft tissue volume is more desirable than more bone volume.
Local conditions like periodontal disease, trauma, teeth infections or sequelae may lead to insufficient bone volume of the alveolar ridge and compromise the outcome of the implant treatment. A bone augmentation of the alveolar ridge is then necessary to allow implant insertion into sufficient bone and in a favorable position according to the prosthetic planning. However, decision should be taken whether it is possible to insert the implant simultaneously with bone graft or bone graft first and implant insert later and what kind of bone grafting (BG) is better to be used?
Autogenous bone is still considered as the gold standard, especially for large alveolar ridge augmentation. It presents essential biologic qualities and properties such as osteogenesis, osteoinduction, and osteocondution. In comparison, allografts, xenografts, and alloplastic materials used in implant dentistry possess only the property of osteoconduction.
Autogenous bone block grafts, suitable for two- or three-dimensional reconstructions of alveolar ridge defects, can be harvested from intraoral sites such as the retro- and paramolar area (external oblique ridge) or the mandibular symphysis (chin area). These grafting techniques requires at least 2 surgical procedures one for bone grafting and another one for implant insertion.
The biologic concept of autogenous bone grafting or the split bone bloc (SBB) or “Khoury’s shell bone graft technique” usually requires 3 to 4 months for bone graft to remodel and to be ready for implant insertion and another 3 months for the osteointegration to take place enabling Implant loading with the prosthetic reconstruction.

Minimal Invasive (MI) Autogenous BG with Simultaneous Implant Insertion
However, not all implant site tissues atrophy requires these major procedures. The reconstruction of small or limited bony defects is possible with locally harvested bone chips and rigid bone core from the implant bed preparation site, using implant drills and trephine burs. This MI approach allows, in most cases, implant insertion simultaneously with autogenous BG and consequently reduce the hole treatment time to only 3 months without the necessity for a second bone harvesting site, advance surgical skills and additional specialized instruments.
After a midcrestal incision reflecting a mucoperiosteal flap and exposing the alveolar crest, the bony defect is explored to determine whether a bone core augmentation with simultaneous implant insertion is appropriate. An important criterion is that the implant must be fully placed inside the bony contours. The bony contours is determined through the volume and shape of the bone of the neighboring teeth and through the bony walls of the implant bed.
The implant bed preparation is started with a trephine bur (offering inside and outside irrigation) and at the same time harvesting a bone core graft about 10 mm in length. Care is taken to achieve sufficient cooling with physiologic serum without heavy pressure on the trephine bur to avoid high temperatures and subsequent thermal damage and bone burning.
After trephine drilling, the core is removed with a core removal instrument. If the core is retained in the trephine bur, a special instrument is pushed into the inner side of the trephine sleeve after unlocking it from the handle of the bur to remove the core from the trephine cylinder (Trephine Ejection Kit By Prof. Dr. Fouad Khoury, Meisinger). The implant bed preparation to the definitive length and width are continued using the original implant system burs under low-speed drilling (< 80 rpm) without irrigation for the collection of additional bone chips. In cases where insufficient bone chips are obtained from the socket, more bone chips can be harvested with a bone scraper from the neighboring area. The implant is inserted inside the bony contours, and the exposed threads are covered with bone chips. The bone core is then adjusted to the defect on the buccal or palatal side, or both, and stabilized through compression with the heads of microscrews (The Bone Management® Micros Screw System Meisinger) screwed in local bone near the core. Pressing of the bone core with the microscrew against the implant body provided a good primary stability. In some cases, depending on the volume of the bony defect, two or more cores (harvested from other implant beds) are necessary to reconstruct the whole bone deficit. Remaining gaps between implant, bone core, and implant bed are filled with autogenous bone chips. No bone substitute materials or membranes are needed. The flap is repositioned and the wound is closed with tension free sutures after a releasing incision is made.







During all these procedures, soft tissue managements are very essential and goes in parallel before, during, after bone grafting, implants insertion and even prosthetic reconstructions. These soft tissues managements are considered to be one of the most important Keys for the success of the prementioned bone grafting procedures.
Conclusion
The use of autogenous bone blocks following Khoury’s biologic concept of bone grafting to reconstruct large bone defect of the alveolar crest for implant treatment, has proven to be successful over more than 10 years after implant loading. However, this procedure requires a second surgical bone donor site, two surgical procedures one for bone grafting one for implant insertion, several soft tissues management, relatively long treatment time comparing to traditional implant treatment with minimum of 7 months until the final prosthetic reconstruction, and an advance highly expertise surgical skills with a progressive learning curve from the operator.
For the beginners in implant treatment, the use of autogenous bone core harvested locally from the implant site, present an easy and minimally invasive treatment for the reconstruction of small bony defects with simultanous implant placement. It requires only one surgical operation for bone core harvesting from the implant bed site simultaneously with implant insertion and bone grafting. A second surgical procedure is required for soft tissue management during the second stage surgery of implant exposure after only 3 months. Additionally, this technique reduce considerably the cost and the treatment time comparing to the other techniques using biomaterials covered with membranes.
To Learn the Techniques Mentioned in this Blog.. Click Here